Patients & Researchers Accelerating Cures
HealthTree unites patients and researchers through cutting-edge technology so they can work together to discover lifesaving treatments for diseases.

Our three pillars of support provide comprehensive patient solutions
Lifetime Support
and Education

Patient-to-Patient
Connections

Powerful Patient
Portal

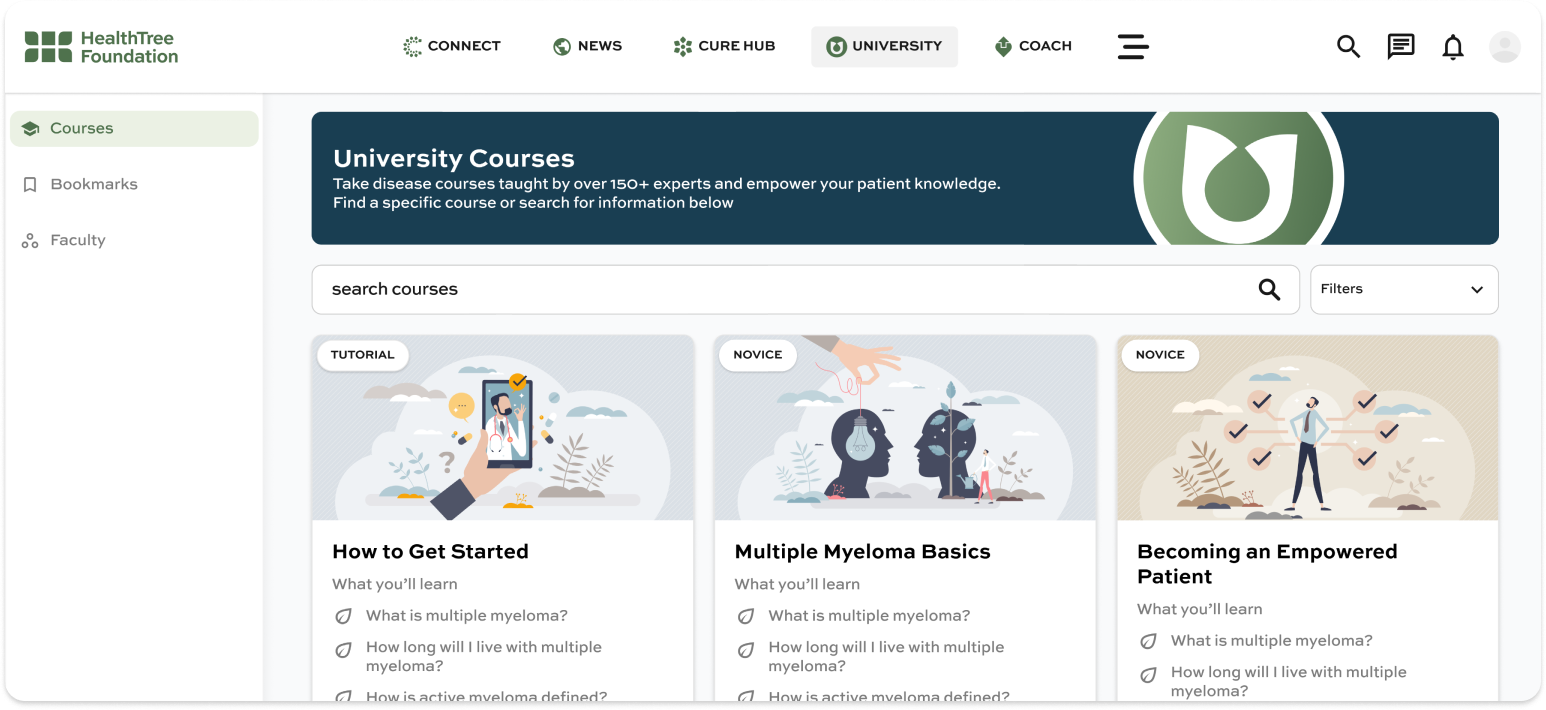
Lifetime support and education
Your brighter tomorrow starts today with free patient education resources
"HealthTree is a unique and fresh approach to gathering patient supplied data and making it available across the spectrum of healthcare professionals, researchers, and fellow patients. "

TINA AND JIM BARDEN
Myeloma and MGUS Patients
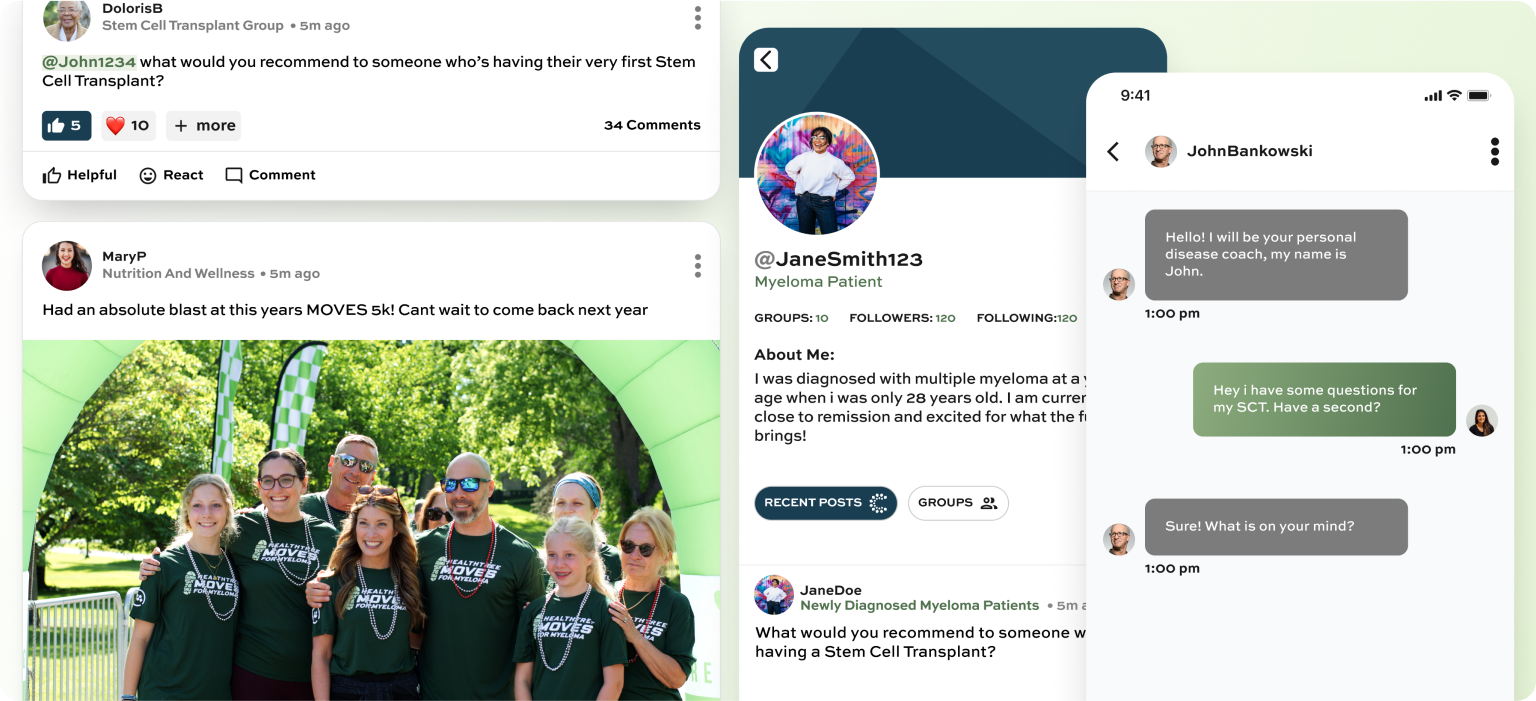
Meaningful patient-to-patient connections
Find a community of patients who care
"The underserved patients will live much longer if their doctor use HeathTree to guide their treatment plans. This is the most useful tool ever developed to bring the most current individualized treatments. "

GARY PETERSEN
Myeloma Patient Advocate
Powerful Patient Data Portal
HealthTree Cure Hub helps you navigate your disease by tracking your labs and so much more
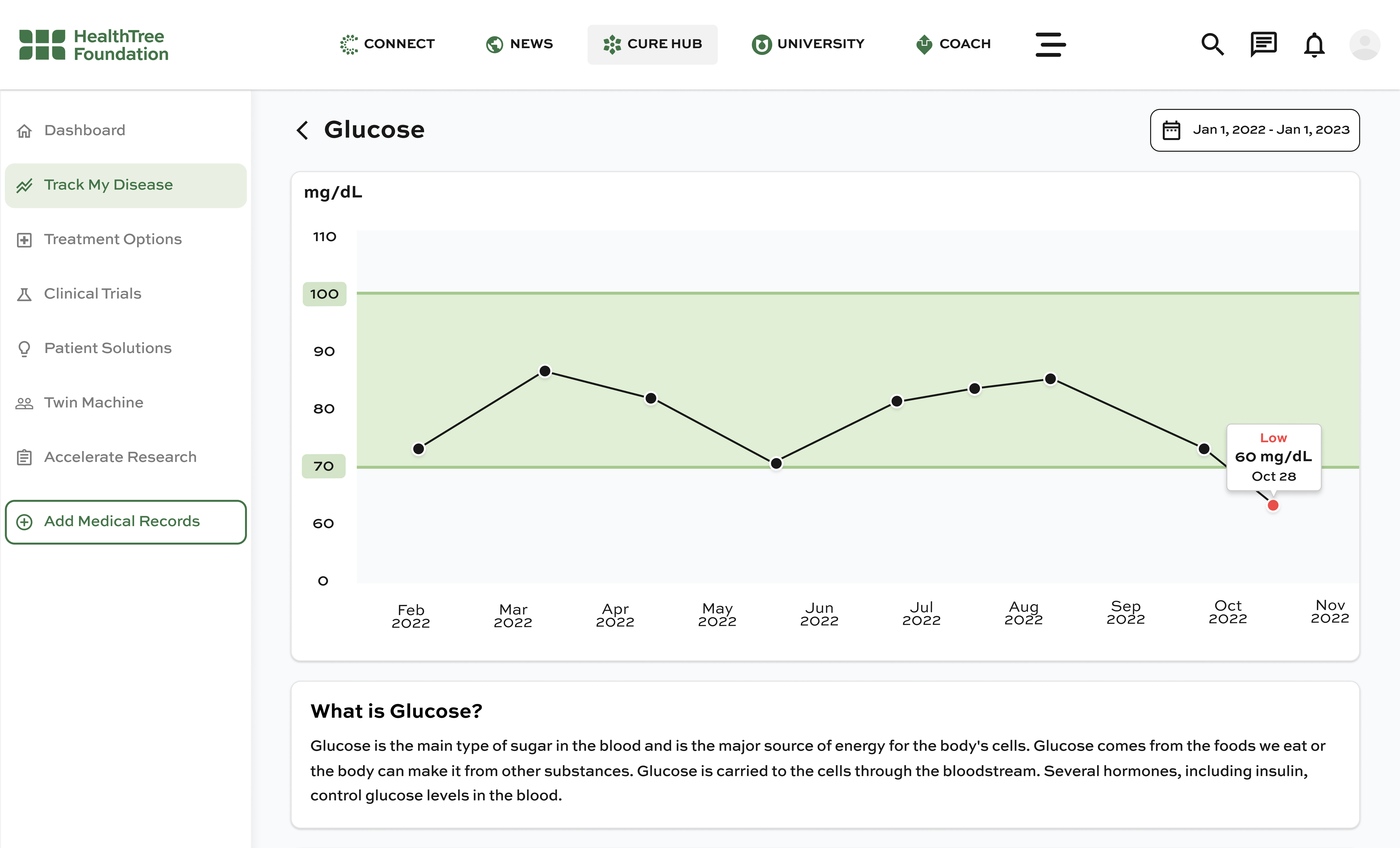
"HealthTree brings into one, easy-to-access place my medical history, my treatment history and my test results, making it easy for me to prepare for doctors’ visits and accurately share my experience with others. "

COURTENAY THOMPSON
Myeloma Patient
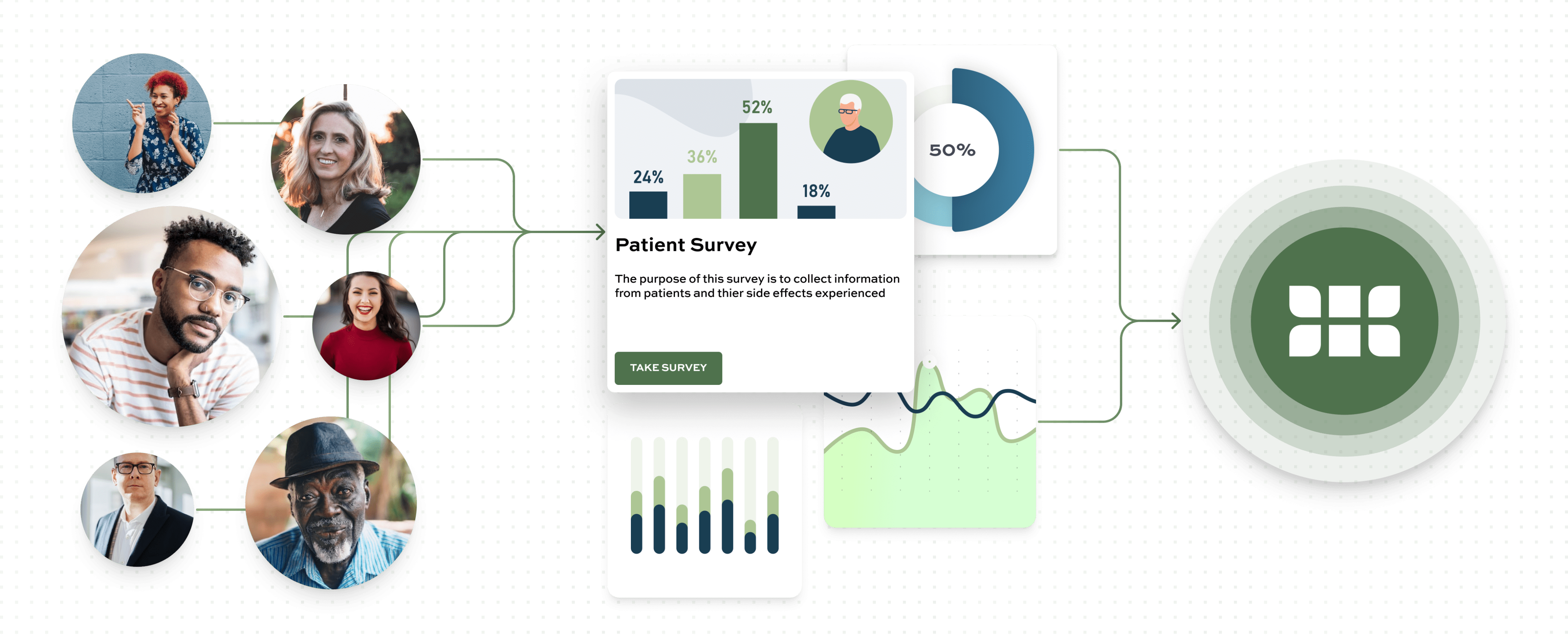
Become part of the cure team by helping researchers discover insights faster
In HealthTree Cure Hub, your data and researchers' expertise combine to shorten the breakthrough time from years to days; every second counts
"HealthTree has created a unique opportunity for patients to empower this work to really make the difference by putting in their own data into HealthTree Cure Hub"

DR. IRENE GHOBRIAL
Myeloma Specialist
Get involved today!
At HealthTree we're on a mission to accelerate cures. Here's how you can help:
Donate to HealthTree, a nonprofit organization
Our core mission is to provide as many patient resources possible to any and all underserved communities in the US and eventually worldwide.
Join the network trusted by thousands of patients worldwide

Download the mobile app to make it easy to access all the benefits HealthTree offers. (Coming Soon)

Track your labs, genetics, and more from all of your facilities in one convenient place
Find life-saving clinical trials perfect for you automatically
Gain free access to step-by-step patient guides
Get on-demand help from our patient navigators
Find a free patient coach for all your needs
Find a community, ask questions and share your story with others
Learn from over 200+ specialists
Join events, chapters and listen to expert podcasts
Stay up-to-date on disease news and breakthroughs
Participate in life-saving research